Your Questions
Fees, Conditions, Coronavirus?
How do I contact you?
I provide a personalized service and have a support team who take calls. To contact my office please call 01727 863447 (0900-1730). If you have had surgery please contact the hospital where you were treated.
Are you seeing patients face to face & operating?
I am seeing patients for face to face consultation and also operating. Where possible, I recommend that the initial consultation is done remotely by telephone or video conference.
If you are having difficulty arranging a consultation with the hospital of your choice please call 01727 863447 (0900-1730) for assistance to see me.
Should I wait for my treatment?
The coronavirus pandemic is no longer classed by the WHO as a global health emergency, but has not been declared over.
My focus is on whether surgery is indicated. If so I will go over the evidence and outcomes regarding treatment and what is known about proceeding in the coronavirus era. And I will develop a plan to address this at the right time and with the least disruption to your home, leisure and work-life.
Should I have surgery now?
If you have red flags (weight loss, trauma, fever, neurological decline, balance, incontinence, sleep disturbance, upper back pain are under 20 or over 55) then you must seek advice.
If you do not have these but you can tolerate your symptoms it may be reasonable to self-manage. Whilst managing, I would urge you to use the time to improve your fitness level and reduce any excess weight. Patient outcomes during the pandemic are greatly improved if you are fit and have a healthy weight.
What is the "new normal"?
I see the "new normal" as having the correct logistic and infection control processes in place (behind the scenes and ostensibly) so that routine surgery can be carried out safely.
You will therefore see measures and checks in place that aim to deliver this. These checks require time and this will be necessary every step of your journey. The scheduling of face to face appointments varies across my hospitals.
As a result of scheduling requirements and pressure on clinic rooms I strongly recommend that you allow at least 1-1.5 hours from the time of your scheduled appointment before making any following commitments. This will provide the outpatients flexibility if there is a need to accommodate you in another clinic room.
What is the outlook for spinal surgery?
Although in the wider community Coronavirus in many quarters is no longer given any consideration, I maintain a mask wearing policy.
The transmission of Coronavirus (Covid 19) is being suppressed with the third lock down, but at a continued high individual and socioeconomic cost and morbidity from non-Covid conditions. Unlike the first lockdown in March provision of elective spinal services continued during the second and now the third Lockdown. However there are ever more stringent criteria that are required before spinal intervention can happen.
The virus has not yet been eliminated and this has far reaching implications for what would have been routine outpatient, daycase and inpatient spinal surgical practice.
The goal is to provide the best outcomes with the least risk and this is achievable with the correct approach and learning at every opportunity.
Is it safe to be seen in hospital?
The fight against Covid-19 requires a multilayered approach. Viruses grow exponentially inside the human body and die exponentially outside the body.
Measures to mitigate the exponential growth inside the body are to stop virus entry and reduce viral load by covid-19 protocols, social distancing, plastic barriers, full PPE "Personal Protective Equipment" (surgical masks and visors during examination), regular testing for Covid-19., correct case mix for surgery, I have been active learning from the experiences of surgeons in Hong Kong, frontline NHS hospitals and authorities on the Spanish Flu and my case mix follows their reintroduction principles. High grade FFP3 masks are used in theatres for aerosol generating procedures, pre and post procedure isolation protocols are in place. Implementing the best practices and approaches that are being used across my 6 hospitals in my Practice. I am swabbed every 7 days for Covid-19 and you will also be swabbed 3 days before any inpatient or daycase procedure.
Measures to accelerate the exponential death of the virus outside the human body include the basics: 6 point hand washing, education on general hygiene (carrying, using and disposing of tissues and face masks responsibly), designated cleaning time between patients, provision and use of hand gels and sanitisers, and the correct set up of outpatient services and scheduling of face to face consultations.
When did the Boris' Deal with the Private Sector end ?
It has ended but the effects remain with a backlog of NHS elective cases.
It has been anticipated that the NHS would operate solely from NHS sites from 1st January 2021. However the third Lockdown put pressure on the Private Sector which was still supporting the NHS effort against Coronavirus (Covid-19) .
This process started in June 2020. Elective activity has resumed across my hospitals, however some sites have a larger ongoing commitment to provide ongoing support to the NHS. This is affecting investigation capacity, bookings and the complexity of surgery that is available. Your overall fitness will be a factor in whether you will be a candidate for intervention during the pandemic.
How long is my appointment?
As a general guide, I will be able to address the important clinical issues in 15-20 minutes. Particularly complex cases may require 30 minutes. No-one likes to be kept waiting and no one likes to leave with unanswered questions, so if your case is particularly complex, such as a second opinion or you have had tests performed elsewhere please call 01727 863774 so appropriate time can be allocated.
Consultation Fees?
My professional fees are in line with the major medical insurers. The guide range you will need to have reimbursed is £100-£275 for your consultation. Where your policy has an excess you will be asked to make up any shortfall. Similarly if you are funding your own treatment. Additional care such as out patient procedures are not included and similarly any items not covered by medical insurance.
How do I make payment?
Payment is made at the time of clinic by debit or credit card (VISA, Mastercard and AMEX). My preference is for debit cards, but the choice of card is yours.
What are your terms and conditions?
All patients are required to be responsible for settling the full cost of treatment. The hospital will take a swipe of your card details. These are not passed onto me and cannot be used to settle your account with me. I will therefore also ask for these details as a back-up for your insurer in the event that the cost of treatment is not settled by your insurance company. If for any reason it is necessary to recover monies owed, all treatment received will default to 150% of the self-funding rate.
Are you fee assured?
I offer fee assurance to select major insurance companies, and not all of my treatments, procedures and surgeries can be accessed with insurance. It is likely that your policy will have a payment limit, or restrictions on the hospitals you can be treated at, there may be further restrictions on the number of consultations, anaesthetists, treatments and locations that are available. If you exceed their limits or terms you will transfer to my standard fees.
Independence?
I am a fully independent spinal surgeon in full time Private Practice. I offer the treatments that I feel will provide you with the best recovery based on rigorous history and examination, special investigations and my assessment of the medical evidence. Please bring copies of any articles, or research that you would like me to refer to at your appointment.
I need an appointment but your clinic is full?
If you are having difficulty getting an appointment, please call my office direct on 01727 863447 and I will find space for you to be seen.
Can I see you and have a scan the same day?
Yes. I provide an all in one package: Initial consultation, MRI, and Follow-Up consultation. Not all medical insurers cover this service. Please call 01727 863447 for details.
Can I have a teleconsultation?
Yes. And during the coronavirus (Covid-19 pandemic) these are being offered by telephone and video. Teleconsultations can be made by prior agreement. Not all medical insurers cover this service and it is offered on a case by case basis. Please call 01727 863447 for details.
Which hospital should I go to?
I offer the my services across all my clinics and hospitals. I consult at the Saxon Clinic Milton Keynes (BMI Group); the Spire Harpenden; Spire Bushey Diagnostic Centre; Pinehill Hitchin (Ramsay Group); OSD Healthcare; Hemel Hempstead and The Clementine Churchill. The range of treatments is tailored to the facilities at my venues
What should I bring to my consultation?
Please bring your insurance details: Insurer, Membership Number, and Authorisation number. A valid debit or credit card, referral letter (if required), and copies of your test results. If you have been investigated at other hospitals and would like me to collect images, to ensure they are available in advance please contact 01727 863447 for advice.
I am happy to see you without a referral letter. However, if you are being referred by your insurer please check with them that they are also happy for you to be seen without one.
Which Insurers are you with?
I work with all medical insurers where you pay my invoice directly and reclaim from your insurer. And I work with select medical insurers where they are paying your invoice to me on your behalf.
Which professional bodies are you registered with?
I am a member of the British Association of Spine Surgeons; Fellow of the Royal College of Surgeons; Member of the North American Spine Society and Independent Doctors Federation. The Federation is recognized nationwide as the voice of independent doctors in all matters relating to private medicine, education and revalidation.
Intervention Fees?
The total cost for treatment is made up of hospital, surgical and anaesthetic fees. For injections the total cost can vary as a guide from approximately £1000 to £4000 for injections £7500 to £10,500 for surgery. Factors that affect this include use of an outpatient facility, length of hospital stay, risk, medical indemnity (the cost of insuring your procedure), number of procedures, complexity, the use of spinal instrumentation i.e. metal implants (is additional), special equipment, physiotherapy/rehabilitation packages and treatment location. I will provide you a letter detailing my charges before you begin treatment.
Children
Do you see children?
Yes. I have had comprehensive training in the wide range of paediatric spinal surgery. This was rounded off with a 12-month Fellowship at Great Ormond Street Hospital and a visiting International Scholarship to the Children’s Hospital of Philadelphia.
Do you operate on children?
I provide an out-patient only service for children from age 13 to those approaching adulthood. The hospitals where I practice are increasingly focusing on adults, and so if surgery is indicated I have established routes of referral to appropriate specialists.
My child has back pain what can be done?
Back pain in children is significantly less prevalent than in adults. Despite this most conditions can be managed without surgery. If this is not settling over a reasonable time frame it warrants clinical assessment.
What are growing pains?
This diagnosis may be made once appropriate tests have been undertaken to exclude common paediatric conditions. It is characterized by non-specific pain during growth and is a self-limiting condition.
My child has a deformity will surgery affect growth?
The spine has three periods of growth: infantile, juvenile and adolescent. The type of surgery offered depends on the child’s stage of development. A common indication would be to control the deformity such as scoliosis. The goal will be to allow the spine, lungs and thoracic cage to develop. Bracing can be considered in certain cases. Despite this treatment, some curves progress. The treatment options include fusion of the spine and operations without fusion (“growing rod technology”).
How much height will be lost if I have surgery?
A simple rule for height loss in a growing child is that the loss of height (in cm) for a particular fusion length is equal to 0.07 X number of segments fused X number of years of remaining growth.
When does maximum spine growth occur?
The two phases of maximum spine growth are between ages 5 and 10 and 10 and 15. Surgery during these periods requires careful assessment. Whilst at Great Ormond Street I had experience researching a period of 15 years of their growing rod program. On average children are in the program for 5 years and have on average six distractions gaining a height of 4.4cm before undergoing definitive surgery.
Are there alternatives to surgery and fusion in children?
Depending on the underlying problem a deliberate growth arrest may be required, magnetic rods inserted, or VEPTR (vertical expandable prosthetic titanium rib). I was co-author of the Smiley Face Technique which is a non-fusion technique developed to overcome the problems of fusion when managing deformity at the base of the spine and stress fractures. This technique has now been extended to treating select similar conditions in adults. Children can also respond to appropriate exercises and rehabilitation. A simple rule for height loss in a growing child is that the loss of height (in cm) for a particular fusion length is equal to 0.07 X number of segments fused X number of years of remaining growth.
Common Investigations Before Surgery
GENERAL CONSIDERATIONS
Common MRI Findings
What does a disc prolapse look like?
In the back, disc prolapses are one of the most common findings. On MRI scan a prolapsed disc looks like a dark oval structure bulging into the spinal canal on the cross- section view. When it touches a nerve you will feel pain radiating from your back down the leg and this is known as sciatica.
Common MRI Findings
In the coccyx, angulation, bony spurs, subluxations, and high signal change are not infrequently seen. Abnormal fusion can be seen at the sacroiliac joints
Surgery
GENERAL CONSIDERATIONS
When to see a Surgeon?
Most times spinal surgery is not needed. Common spine issues are pain, locking, giving way, weakness, altered sensation, curvature of the spine or difficulty walking or holding items. More pain does not necessarily mean more injury. A surgical opinion is warranted if you are not responding to self-help measures and have significant pain or dysfunction. I will talk you through the options and tailor a plan for you.
What do you mean the pain is not in my back, I can feel it is there?
The pain you experience in your back may in fact originate elsewhere in the body, such as the gall bladder; pancreas; stomach; kidneys; heart; lungs; prostate and gynaecological organs. To ensure that these and other serious conditions are not overlooked or misdiagnosed, a full medical consultation and examination should be undertaken before surgery is considered.
Do I need surgery?
Surgery for a disc prolapse is generally an elective procedure. The decision to operate is individualized. You must carefully study the risks of surgery and satisfy yourself that you have exhausted all conservative options first. If symptoms are intolerable this is an indication for prompt surgery, and if there is progressive neurological decline or for example bladder or bowel problems, urgent spinal surgery may be needed.
Which surgery is best?
Surgery for disc problems causing leg and arm pain has the best outcomes. Surgery for predominantly lower back pain for well selected cases is 65%. Surgery for cord compression has the best outcomes when done without delay. For back, neck, leg and arm pain, the less bones that need fusing the better the odds of success, when you have an anatomical diagnosis.
Risks of Spine Surgery?
General: Nerve Root Injury, Scarring, Dural Leak, Infection, Wound Swelling, Recurrent Disc Herniation, Blindness (rare)
Neck: Recurrent Laryngeal Nerve (Hoarse Voice), Vertebral Artery, Respiratory, Oesophageal Injury, Spinal Cord Injury
Lumbar: Cauda Equina, Acceleration of unrecognized myelopathy, (Retrograde Ejaculation, Catastrophic Bleeding, Abdominal organ injury with Anterior surgery)
Metalwork: Failure of Union, Metalwork Breakage, Malposition, Dislocation of Implant, Problems where the metalwork ends.
I will provide a specific list for your surgery with odds of occurrence.
Preparation for surgery?
Minimise stress in the run up to the operation. Cigarette smoking is associated with poorer outcomes in all spine surgery. If you smoke I will urge you to stop. I specialize in disc surgery and operate on patients with high BMIs. If you can lose weight gradually this will help. However, it is important not to go on a crash diet in the run up to surgery. A well-balanced diet of fresh fruit, vegetables and protein will aid recovery. Attention to weight reduction begins 3 months after surgery.
You will need to stop eating and drinking 6 hours before admission. You may drink water up until 2 hours before your admission. If you are on anticoagulants you may need to stop these and have special injections to provide anticoagulation in the run up to surgery. Pack for an overnight stay. Remember to bring a change of clothes, including slippers, and dressing gown and toiletries. Do not bring valuables.
COMMON INVESTIGATIONS BEFORE SURGERY
Radiographs (X-rays):
X-rays are a very energetic form of light energy that allow us to look through your skin to see structures that contain calcium like bone. X-rays are a good choice to see bony anatomy such as spinal deformity and broken bones.
MRI scans:
MRI scans let us look at the soft tissues which have a high Hydrogen content. The soft tissues of your body are 65% water (H2O) so there is plenty of Hydrogen (H2) to be seen. The MRI forms an image by magnetizing tissues and forming an image in the process. MRI scans are a good choice to see the discs.
CT scans:
“CAT” scans are a high-tech way at looking inside you. They use radiation and require the benefits to be weighed against the risk. They provide me with information that other tests may not. This test conveys precise anatomical detail and eliminates sinister pathologies.
Dynamic MRI:
Conventional MRI scans are taken lying down. One of my research interests is the practical application of dynamic MRI scanning. If your symptoms come on when standing or sitting you may be a candidate for this technique. You can be scanned in your position of pain to maximise the chance of finding the cause.
CT Guided Root Block:
Useful to plan surgery
COMMON OPERATIONS: Back
Lumbar Discectomy/Decompression:
Suitable for:
Disc Problems, Spinal Stenosis
Aim:
This operation is designed to remove part of the disc (or excess bone) that is touching a nerve causing leg and back pain. I do this operation with an operating microscope. A small incision is made in the back over the disc. Fine microsurgical instruments are used to remove the disc material.
Recovery Time:
Typically, you will go home the following day, and return to work at 6 weeks, possibly earlier depending on the nature of your work.
COMMON OPERATIONS: Back: Metal Work
Interspinous Devices:
Suitable for:
Disc problems, Stenosis. These devices are a good option for patients who require more complex disc surgery but wish to minimize their spinal intervention without limiting future revision options or are medically less fit or elderly.
Aim:
This operation is designed to remove pressure from nerves without disturbing the nerve roots that are causing back and leg pain. This technique can be performed using minimally invasive techniques (MIS) or as part of a fusion procedure.
Recovery Time:
You will leave hospital the day after the procedure and can return to work rapidly. I urge patients to use the full 6 weeks to recovery unless you have a strong desire to return to work early.
Lumbar Spinal Fusions:
EXAMPLE OF FUSION SURGERY:
The images show how I treat a stress fracture of the lowest bone in the spine.

On this CT. The bones to the right of the image lie on top of each like roof tiles. The roof tile is disrupted in the lowest image because of a fracture (i.e a broken bone)

The disc space is seen to be distorted and the lower bone has changed to a white colour which can be a sign that this is causing pain.
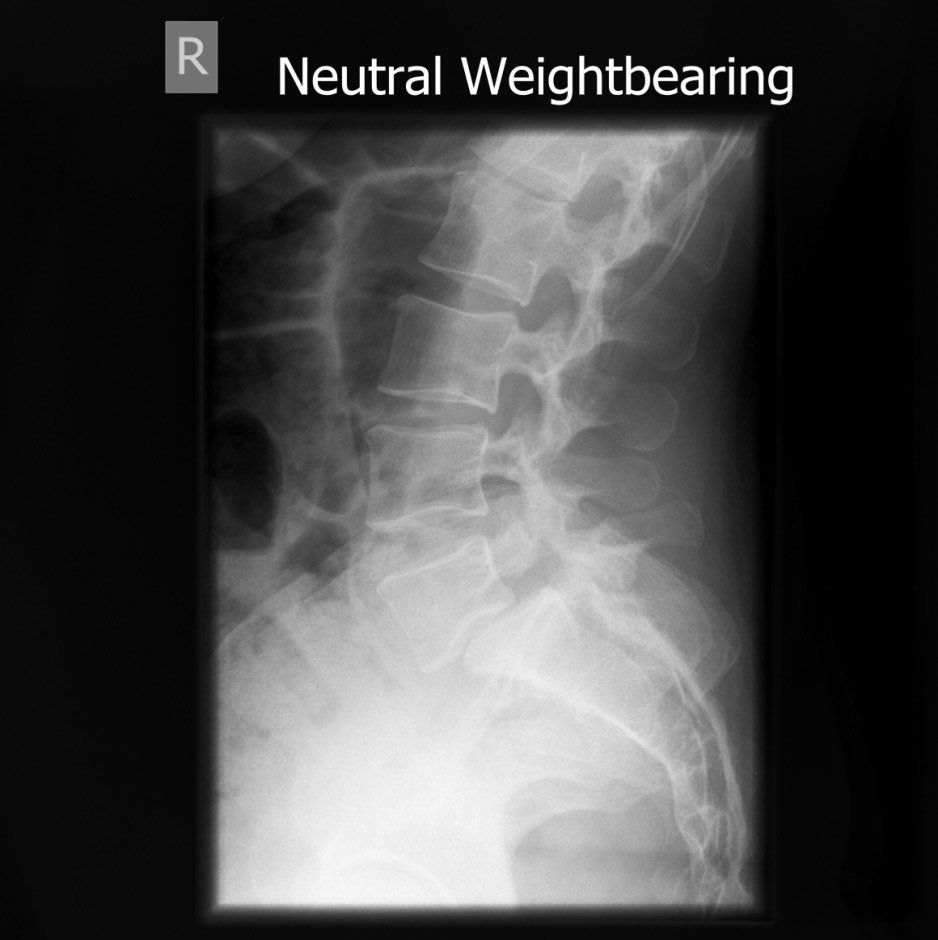
This is the before surgery X-ray showing that the lowest bone has slipped forward.
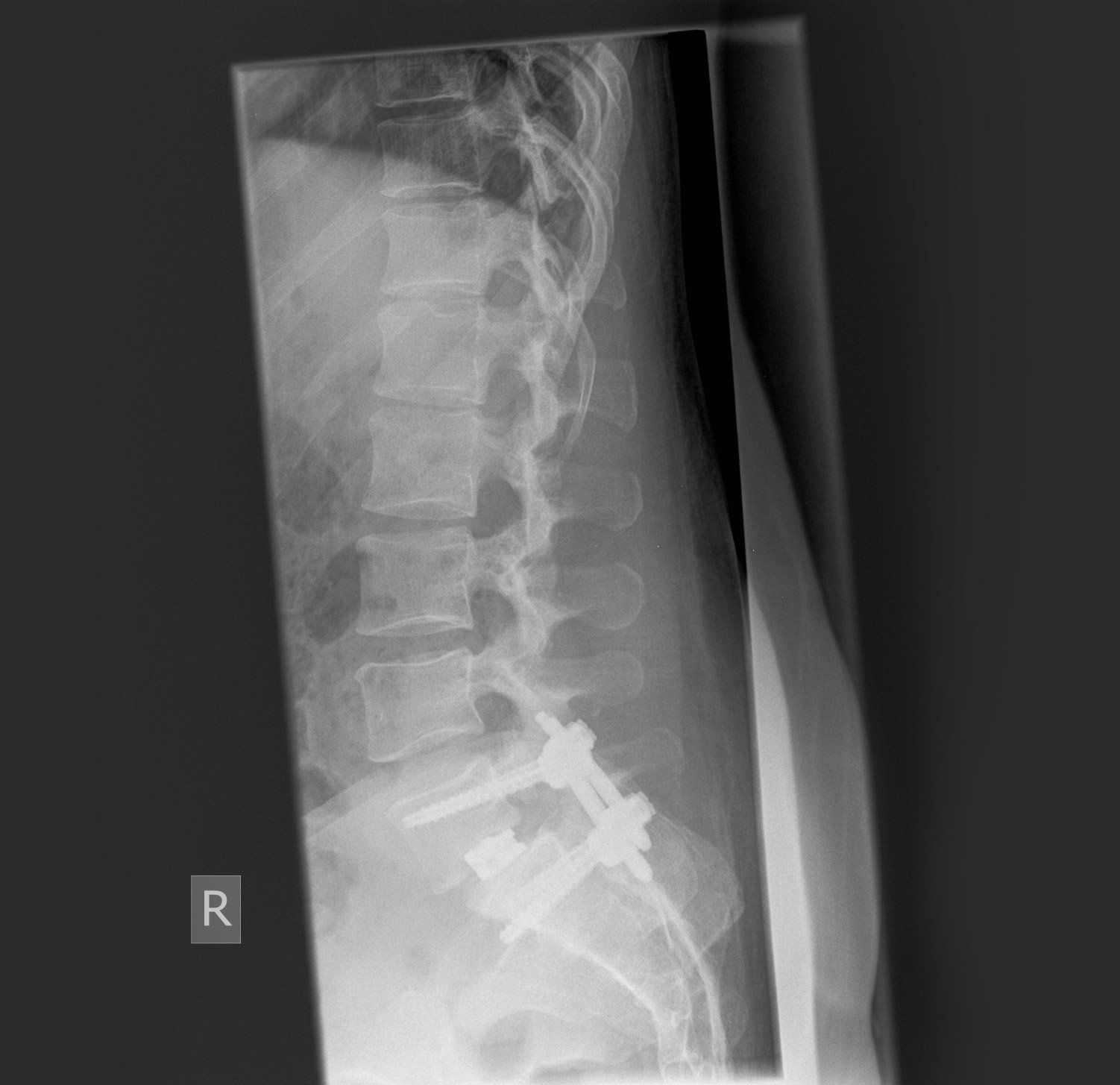
This is the post-surgery X-ray showing that the slip has been corrected and a metal scaffold has been placed into the bones either side of the slip. A cage with bone graft has been put into the disc space to complete the spinal fusion.
Metal work has been put into the spine to allow the spine to fuse to correct the defect and improve pain.
Common Operations: Neck: ACDF
Suitable for:
Neck & Arm Pain, Weakness, Balance Problems
Aim:
This operation is designed to remove pressure from the nerves and spinal cord in the neck that are causing pain and weakness. I perform this surgery using the operating microscope. The aim is to remove pressure from a trapped nerve and cleanout a damaged disc. I then place bone graft in a special cage between the spinal bones to replace the damaged disc to do the fusion.
Recovery Time:
You will leave hospital the following day or two and can return to work in 2 weeks. Pain relief can be immediate following the surgery.
Should I have surgery:
ACDF is an excellent operation to release pressure from a trapped nerve in the neck. If the pain is predominantly in the neck with little arm pain alternatives to surgery should be considered first.
Suitable for:
Neck & Arm Pain, and where a strong desire to preserve movement is needed such as having previous fusion surgery.
Aim:
This operation is designed to remove a damaged disc and replace with an artificial disc. Fusion surgery still remains the gold standard
Recovery Time:
You will leave hospital the following day or two and can return to work in 2 weeks. Pain relief can be immediate following surgery.
Should I have surgery:
Cervical Disc Replacements are showing promise but have not been shown to be better than ACDF. They can be considered where there is a strong desire to maintain movement.
CEMENT AUGMENTATION
Vertebroplasty/Balloon Kyphoplasty
Suitable for:
Osteoporotic spinal fractures and certain tumours
Aim:
Viscous (Sticky) cement is injected into the spinal bones using a special delivery system to strengthen the bones. Kyphoplasty aims to restore bone height. Vertebroplasty aims to integrate directly with the bone.
Recovery Time:
An overnight stay is usual and return to work at 2 weeks.
Should I have surgery:
All the risks of surgery including heat damage of the spinal cord by cement
REVISION SURGERY
Revision surgery present challenges that are not present with primary surgery. You may have altered anatomy, scarring or problems with the metalwork which typically happen above and below where the spine fuses. I provide reasoned clinical decision making to move things forward.
HOW TO AVOID SURGERY
What can I do to avoid surgery?
Between the ages of 25-40 the back starts to show the signs of normal aging. Up to 80% of adults will suffer from back problems every year. The majority will settle within 6 weeks. If you are a sufferer your chances of a further attack in the year is 50%. Being aware of everyday risk factors lessons your chances of further attacks but will not bring your odds to zero. Sitting down puts the most pressure on the spine, and bending forwards whilst twisting is the worst position for the lower back. Health care workers are at the most risk followed by wholesalers, retailers, and labourers.
What are the general risks for my back?
Menstruation, diabetes, hormone disorders, commuting more than 20 miles, smoking (damages the arterial flow to the disc ligaments), chronic cough (increases pressure in discs), static positions, psychological factors (are very real), depression, bereavement, divorce, moving house, HGV driving, using a weight lifting belt when not using weights are just some of the things to be aware of.
Pain Management
GENERAL CONSIDERATIONS
What is pain management?
This is the use of non-surgical pain management techniques that can include medication or relatively invasiveness X-ray guided techniques to reduce pain to manageable levels.
What are the common causes of back pain?
Non-specific back pain, ligament injury, tendon muscle strains, disc prolapses, and spondylosis are all common.
I am in severe pain something serious must be wrong?
There is normally a direct relationship between pain and tissue damage. This relationship breaks down when pain becomes chronic. You may have severe pain and a normal MRI scan, or multiple problems seen on MRI scan and have no pain. Most back pain is self-limiting. However, if the pain has persisted more than 6 weeks or you have red flags a visit to your GP is indicated to be fully assessed and exclude treatable causes.
Should I Keep Moving if I am in pain?
Stay active! Gently coax the spine through the pain. It is understandable to be apprehensive but in most instances the pain will reach manageable levels in a day or two
Is my back pain serious?
Red Flags: The following symptoms warrant medical investigation. Weight loss, Trauma, Fever, Weight Loss, Neurological decline, Balance, Incontinence, Sleep disturbance, Upper Back Pain, under 20, Over 55.
Why do I have back pain but a normal MRI Scan?
Acute non-specific back pain is one of the commonest causes of lower back pain. It will affect 80% of the adult population at some point in their lives. Symptoms of stiffness will generally resolve within 6 weeks. In non-specific back pain the MRI scan does not show a clear anatomical site for pain. This does not mean that there is “nothing wrong” but an indicator that surgery will be unsuccessful.
Chronic non-specific back pain is recurrent bouts of non-specific back pain. The onset is unpredictable, it can happen early in the morning, you may be unable to stand, sit or straighten. Recent NHS guidelines and pressures on hospitals have reduced the options for managing this condition.
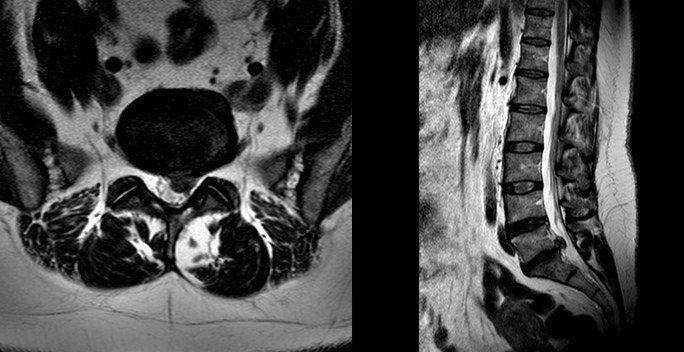
What does a disc prolapse look like?
The pictures above are of an MRI scan showing a prolapsed disc. The dark oval structure in the centre is a disc and the bulge coming off the base is the “prolapsed disc” protruding into the spinal canal on the cross- section view. In the image on the right the disc prolapse can be seen as a circle behind the spinal bones. When it touches a nerve you will feel pain radiating from your back down the leg and this is known as sciatica.

When do I need a re-scan?
The images below show a resolved disc prolapse. There is no longer black material in the spinal canal. Whether you need a new scan will depend on how you respond to treatment, clinical assessment and if it is felt you may benefit from an operation.
Can my disc prolapse heal itself?
Yes. The body has a remarkable capacity for repair. This prolapse resolved within 3 months. The body shrinks the disc by absorbing water, when this process is complete your pain will improve. The majority of discs will improve given long enough. My role is to guide you through the options, and step in if your life is on hold and waiting is unacceptable you may be a candidate for surgery on the lower back.
MRIS
Understanding your scans
The MRI report is written to convey to other doctors what the radiologist has seen, without the radiologist having seen you. Common terms that are encountered are
Disc Diseases - “Bulges, Extrusions, Herniations, Prolapses, Protrusions, Slips, Loss of height, Dehydration, Dessication, Degeneration”.
Joint Diseases - “Facet disease, hypertrophy”.
Bone problems - “Fractures, loss of height, marrow change, anterolishesis, retrolisthesis”.
Ultimately MRI interpretation requires a comprehensive history and examination by a specialist or generalist with a special interest who has experience managing common spinal conditions. If your pain has persisted for 6 weeks or you have red flags then a visit to your doctor is indicated to provide specific advice.
If you have had a scan organized by another doctor before you see me, please call my office on 01722 863447 so that adequate provision is made before your consultation to retrieve the images if necessary and allocate time to review these.
Prevention
How to avoid surgery
What can I do to avoid surgery?
Between the ages of 25-40 the back starts to show the signs of normal aging. Up to 80% of adults will suffer from back problems every year. The majority will settle within 6 weeks. If you are a sufferer your chances of a further attack in the year is 50%. Being aware of everyday risk factors lessons your chances of further attacks but will not bring your odds to zero. Sitting down puts the most pressure on the spine, and bending forwards whilst twisting is the worst position for the lower back. Health care workers are at the most risk followed by wholesalers, retailers, and labourers.
What are the general risks for my back?
Menstruation, diabetes, hormone disorders, commuting more than 20 miles, smoking (damages the arterial flow to the disc ligaments), chronic cough (increases pressure in discs), static positions, psychological factors (are very real), depression, bereavement, divorce, moving house, HGV driving, using a weight lifting belt when not using weights are just some of the things to be aware of.
Exercises
What are the best exercises for the back?
My interest in exercise physiology began in the laboratories at Oxford researching the effect of endurance exercise on essential body proteins. At the same time, I was a triple jumper and Athletics Blue. I have first-hand sporting and clinical experience of the requirements for a fit spine. Exercises must improve your strength, speed, flexibility, balance and control. They should be modified to gently rehabilitate an injured back. If you have not done much physical activity for a while are an older person a consultation with your GP before you start is advisable.
What Exercises should I avoid?
If the pain has come on because of a particular exercise (s), or you are unaccustomed to exercise: The intensity and frequency of the exercises should be reduced until they reach manageable levels.
Strength
What are the Core Muscles?
The body’s core are the muscles of the midsection, that is the torso, abdomen, lower back, pelvis and hips. These muscles stabilize the lower body whilst you are exercising your arms; and stabilize the upper body whilst you are using your legs. Strong core muscles protect the spine from injury.
What are Core Exercises?
Core exercises have received a lot of attention in the media, often focusing on difficult exercises like the plank and deadlifts. In fact, all exercises which involve supporting your own body weight will significantly improve your core strength.
Speed
Modern life means that without conscious effort it is very easy to spend nearly 99% of the day with minimal exertion. A typical day would be a commute, sitting, and intermittent standing before sleeping. Walking raises the heart rate and activities such as running and cycling will make you sweat. As a guide, activity is moderate if it raises the pulse rate and vigorous if it makes you sweat. Current NHS recommendations are 3 hours of moderate exercise or 1.5 hours of vigorous exercise a week, providing you have checked that you are medically fit with your family doctor. Using a pedometer or exercise tracker to count steps is a good way to start or increase daily movement.
Flexibility
Your muscles generate power by contracting (shortening). The longer they are, the more they can shorten. A stretched muscle will therefore move your spine more efficiently. It is important to stretch by bending forwards and backwards and to the sides. Suitable exercises can be performed lying down or seated.
Whilst lying face down, place palms on floor next to your shoulders and push up to arch your back. Alternatively, kneel down, sit on your heels and stretch your arms out in front.
Whilst lying on your back, tuck your knees to your chest and hold for 10 seconds. or stretch your back over a pillow, or whilst seated over the back of a chair,
Pelvic tilts aim to draw the hips up and straighten out the curve in the lower back to there is no gap between the lower back and the floor.
Rotation of the spine, and hips will allow the muscles on the side of the spine to be stretched.
Balance and Control
Exercises to improve balance include standing on one leg, walking side-ways, heel-to-toe walking are all simple exercises to improve balance and control. Exercises to improve spinal health do not require sophisticated equipment or gym memberships.
Medication
Won’t drugs mask the pain?
The signs and symptoms of serious spine conditions are not masked by over the counter pain killers. Getting on top of the pain aids early recovery. Paracetamol tends to boost the effect of other pain killers that it is taken with. It can therefore be combined with drugs such as Ibuprofen an anti-inflammatory drug. A short period of 1-2 days rest may be needed. However, longer than 2 days of rest will make it harder to get going. If stronger mediation is needed a visit to your GP is called for who may consider Codeine, Amitriptyline or Gabapentin.
Work Environment
Raise the computer screen so that you can see it without bending the head down. Chairs should have wheels and arm rests. Elbows should rest comfortably on the arm rests, bent at 90°. The mouse hand should have a mouse support. The hips should be slightly higher than the knees, so that the legs can do some of the work of sitting. Ideally avoid sitting for longer than 30 minutes.
Allied Health Care Professionals
I work closely with physiotherapists, osteopaths and chiropractors who have a special interest in rehabilitation of the spine. Together we can tailor an exercise program for you and guide you to perform them safely.
The Posture & Shape of the Spine
The spine is an elegant s-shaped structure when viewed from the side. It has 4 regions. The neck has 7 bones and is called the cervical spine. The upper back has 12 bones with pairs of ribs attached to it and is called the thoracic spine. The lower back has 5 bones (sometimes 6) with no ribs attached to it and is known as the lumbar spine. The lowest region is the sacrococcygeal spine. This has the sacrum (strictly part of the pelvis) and the coccyx (tail bone). The bones get bigger as you go down the spine. The structure protects nerves, the cord and the muscles, ligaments and tendons allow movement and supports the upper body. Poor posture and loss of the normal curves is a frequent cause of pain and loss of function.